Welcome to the 2022 Spring Conference Virtual Poster Session!
The authors recorded brief descriptions to enhance their presentation; click the “Download” button and “Play Slide Show” to listen to the description. Email the primary author with any questions or comments by clicking on their name below the poster.
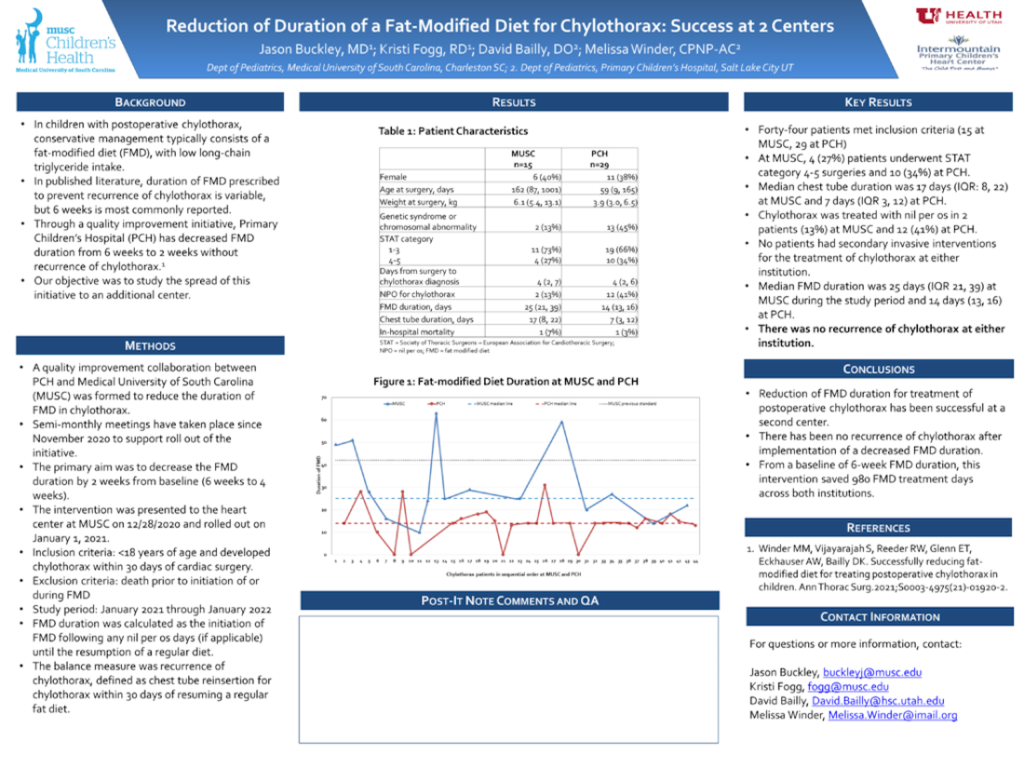
Reduction of Duration of a Fat-Modified Diet for Chylothorax: Success at two centers
Jason Buckley, MD Medical University of South Carolina
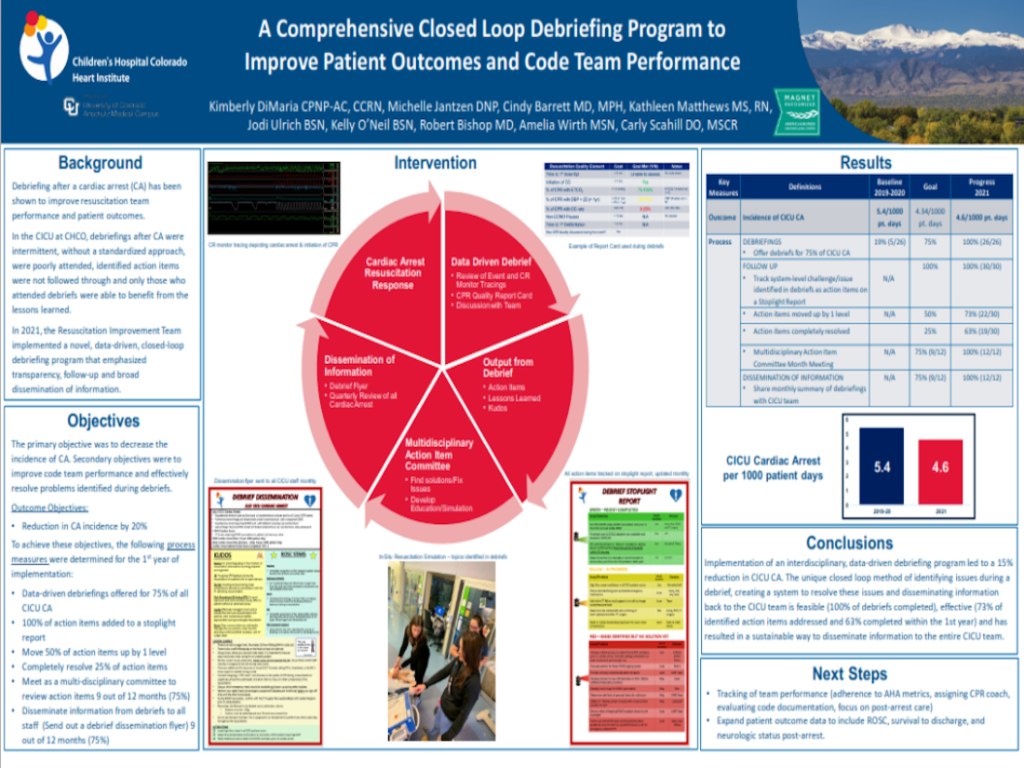
A comprehensive closed loop debriefing program to improve patient outcomes and code team performance
Kimberly DiMaria, CPNP-AC, CCRN Children’s Hospital Colorado
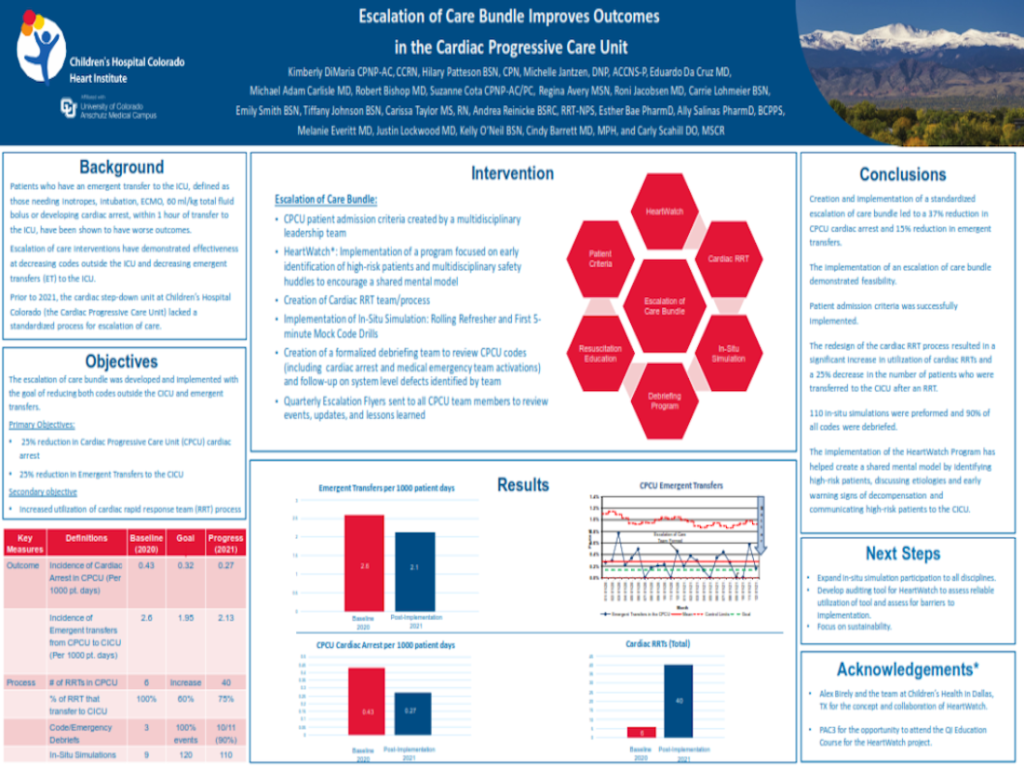
Escalation of care bundle improves outcomes in the Cardiac Progressive Care Unit
Kimberly DiMaria, CPNP-AC, CCRN Children’s Hospital Colorado
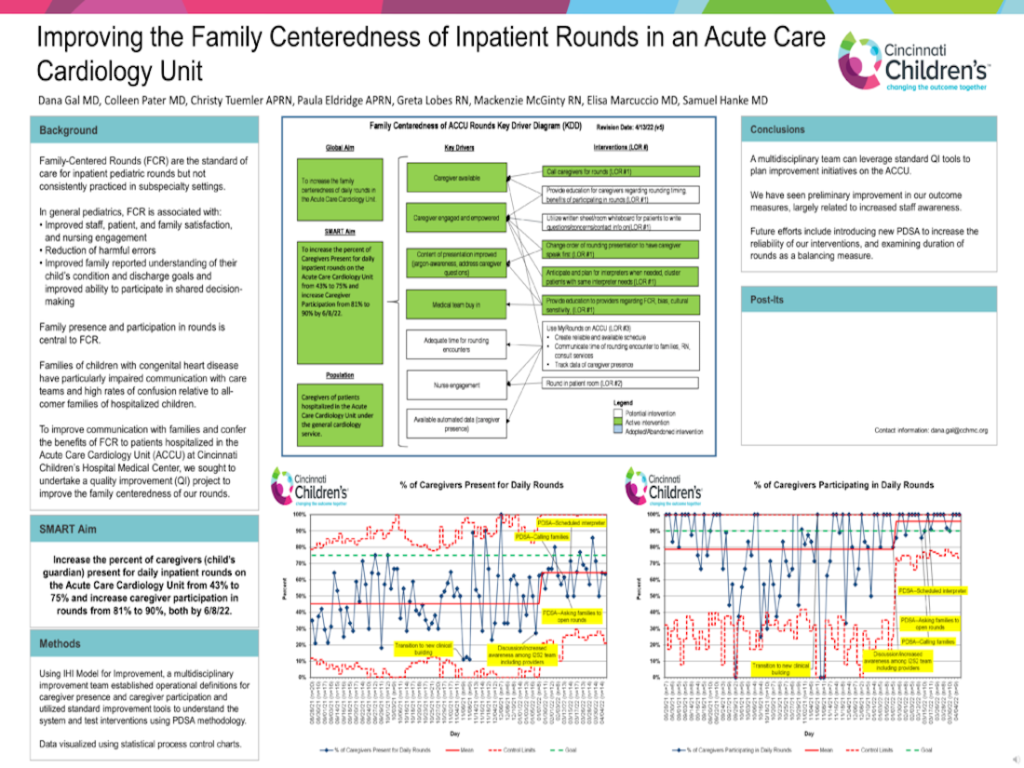
Improving the family centeredness of inpatient rounds in an Acute Care Cardiology unit
Dana Gal, MD Cincinnati Children’s Hospital
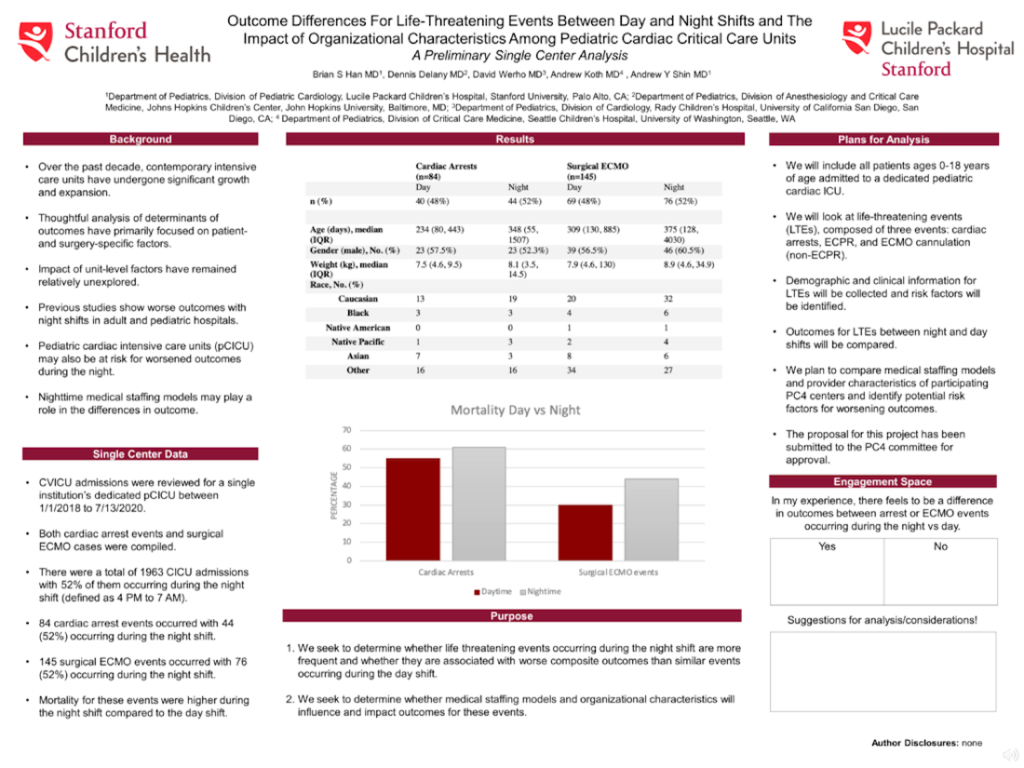
Outcome differences for life-threatening events between day and night shifts and the impact of organizational characteristics among Pediatric Cardiac Critical Care Units: A preliminary single center analysis
Brian Han, MD Lucile Packard Children’s Hospital at Stanford
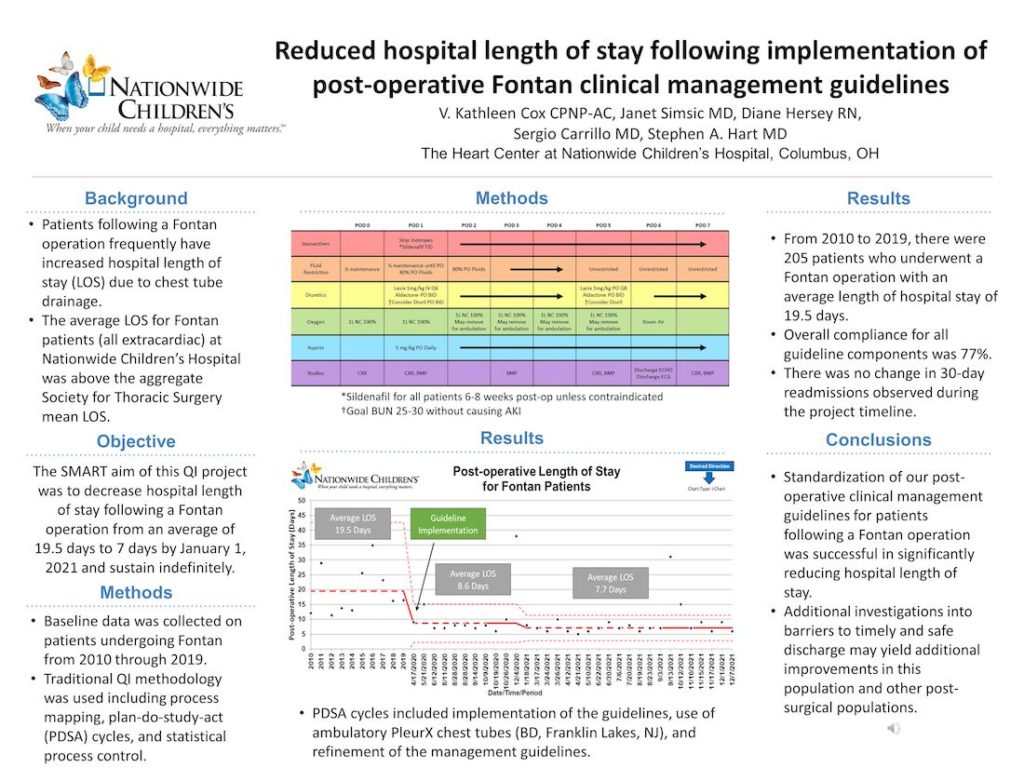
Reduced hospital length of stay following implementation of post-operative Fontan clinical management guidelines
Stephen Hart, MD Nationwide Children’s Hospital
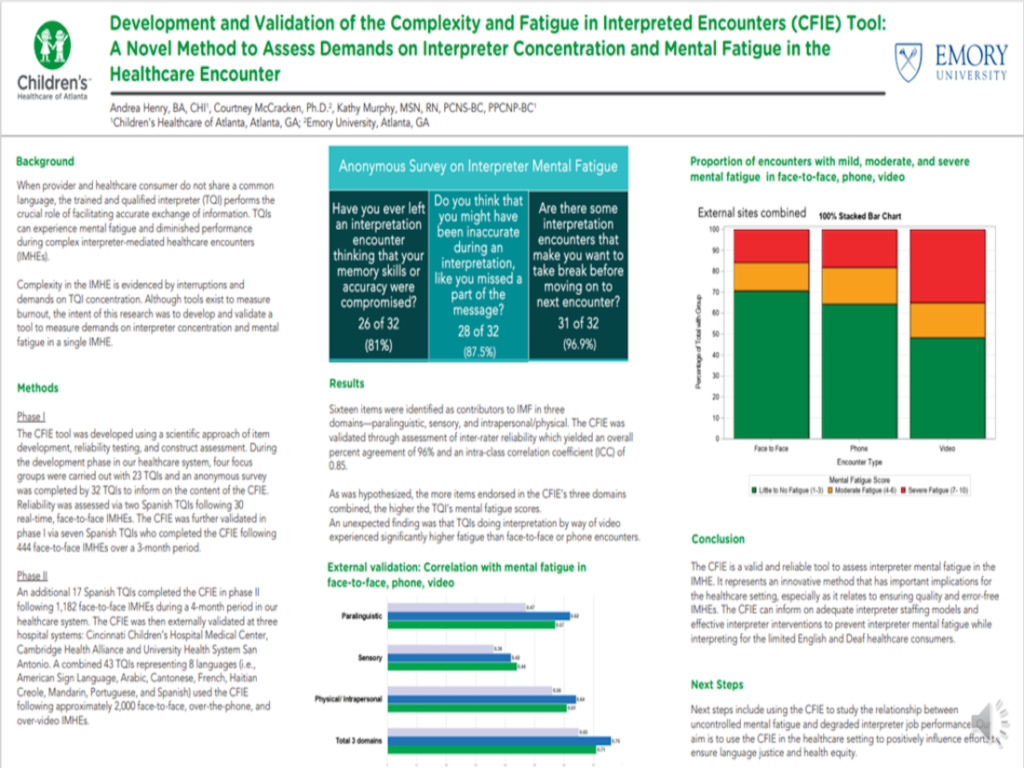
Development and validation of the Complexity and Fatigue in Interpreted Encounters (CFIE) Tool: A novel method to assess demands on interpreter concentration and mental fatigue in the healthcare encounter
Andrea Henry, BA, CHI Children’s Healthcare of Atlanta
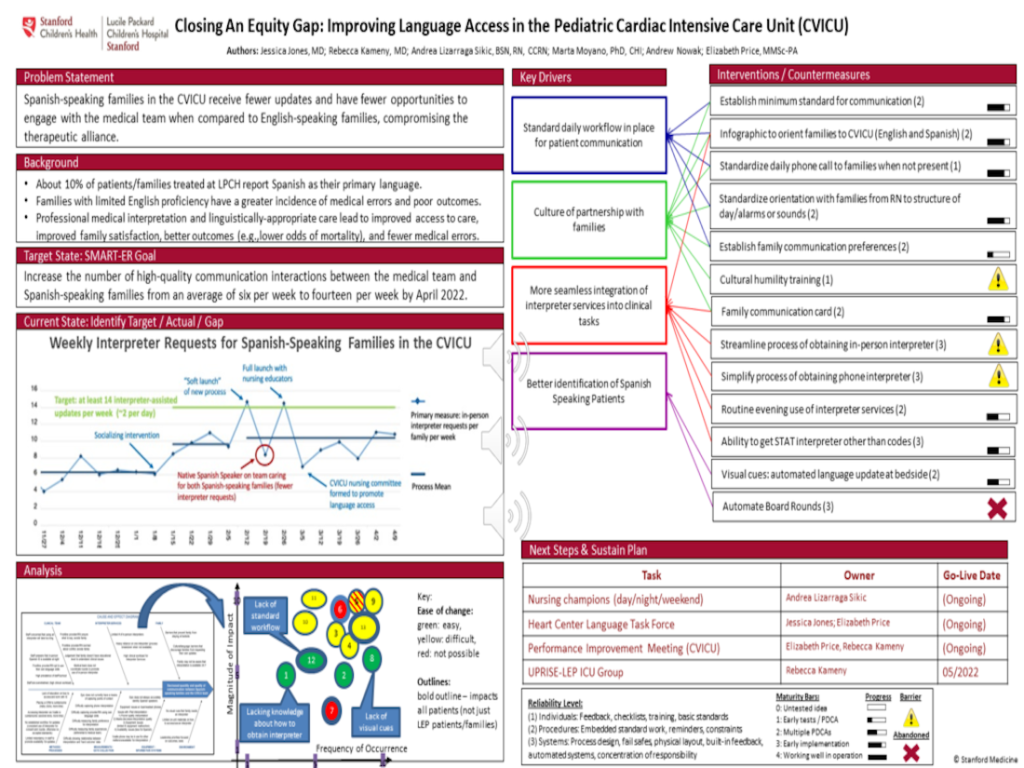
Closing an equity gap: Improving language access in the Pediatric Cardiac Intensive Care Unit (CVICU)
Jessica Jones, MD Lucile Packard Children’s Hospital at Stanford
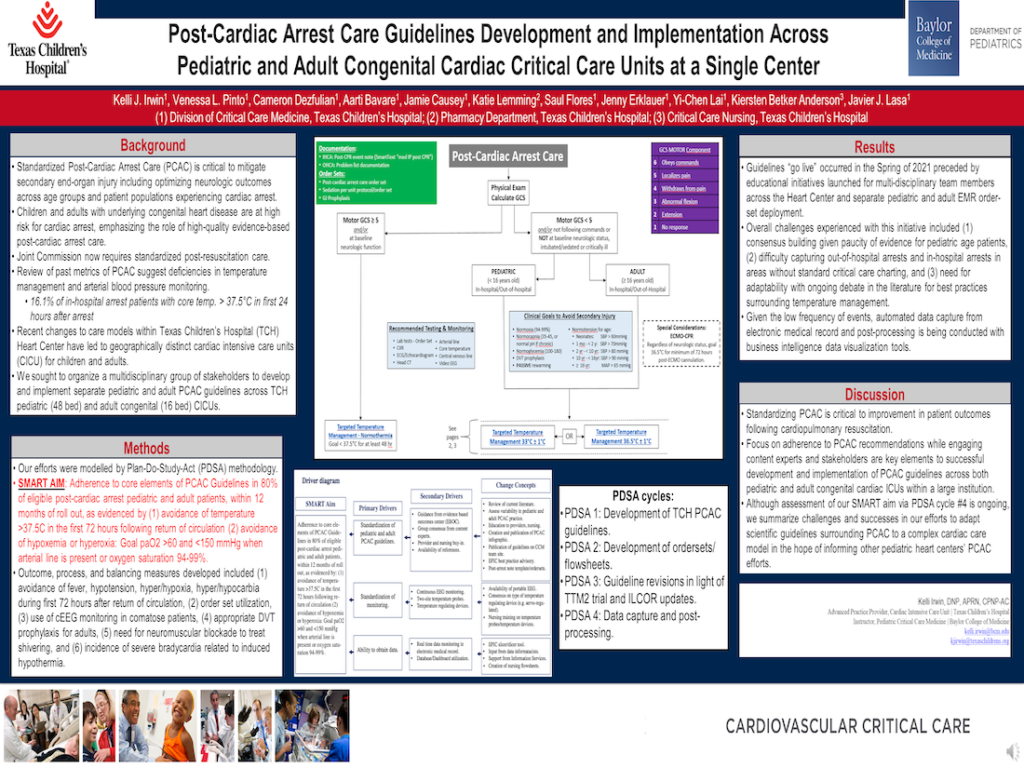
Post-Cardiac Arrest Care Guidelines Development and Implementation Across Pediatric and Adult Congenital Cardiac Critical Care Units at a Single Center
Kelli Irwin, DNP, APRN, CPNP-AC Texas Children’s Hospital
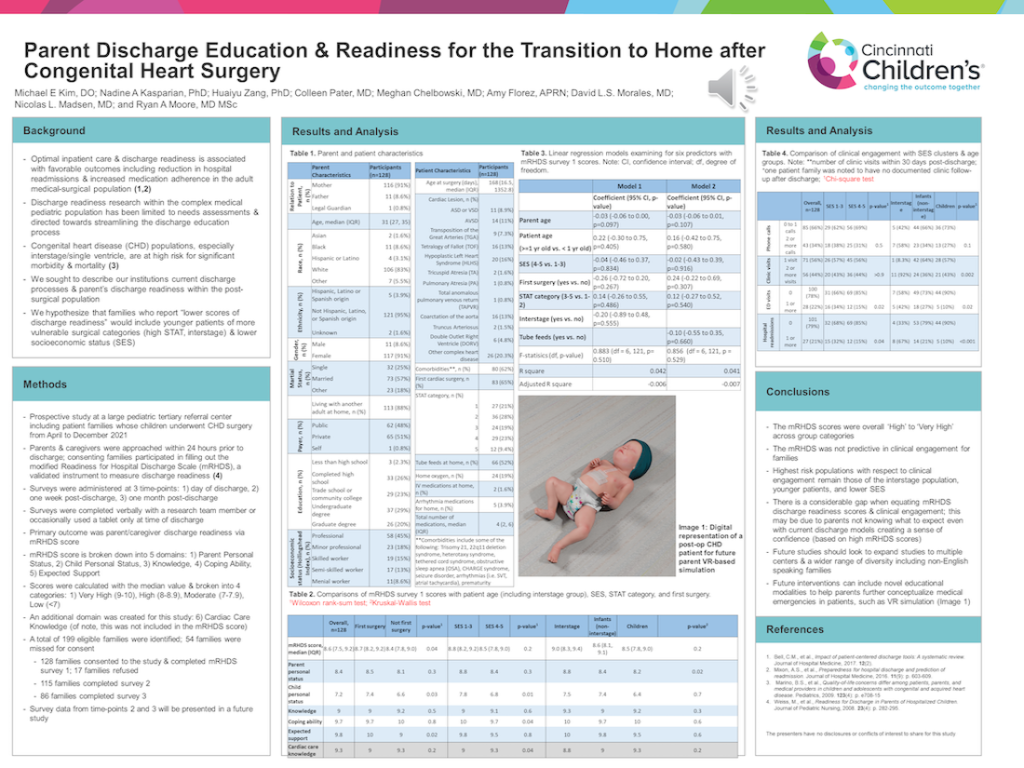
Parent discharge education & readiness for the transition to home after congenital heart surgery
Michael Kim, DO Cincinnati Children’s Hospital
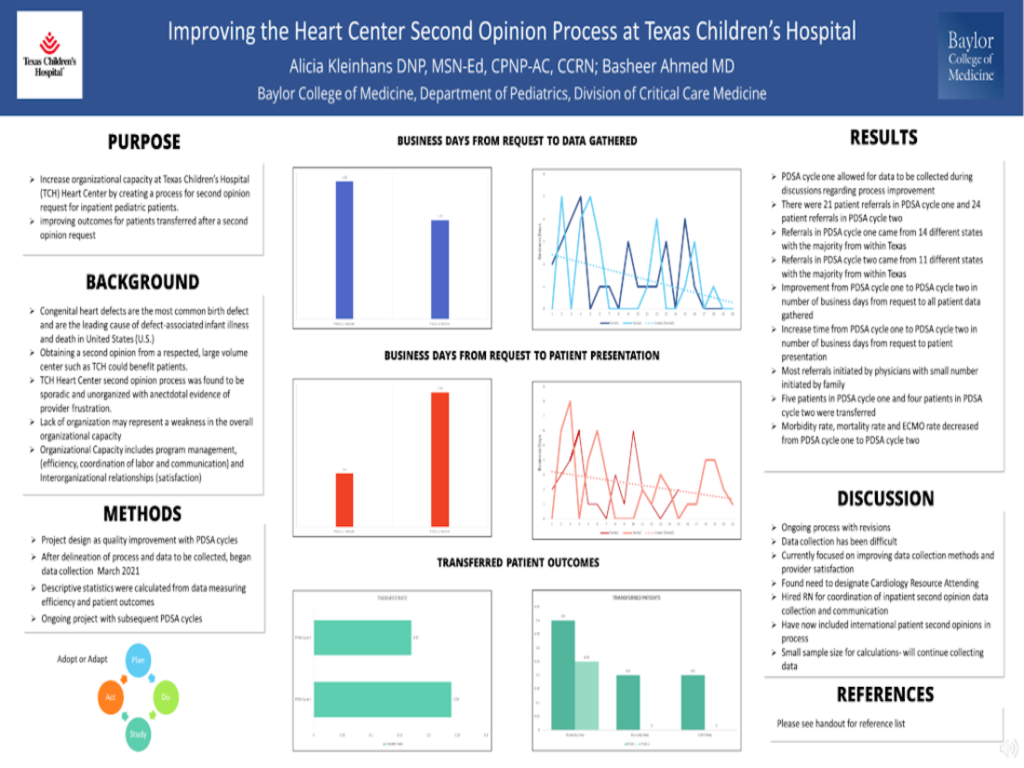
Improving the Heart Center second opinion process at Texas Children’s Hospital
Alicia Kleinhans, DNP, MSN-Ed, CPNP-AC, CCRN Texas Children’s Hospital
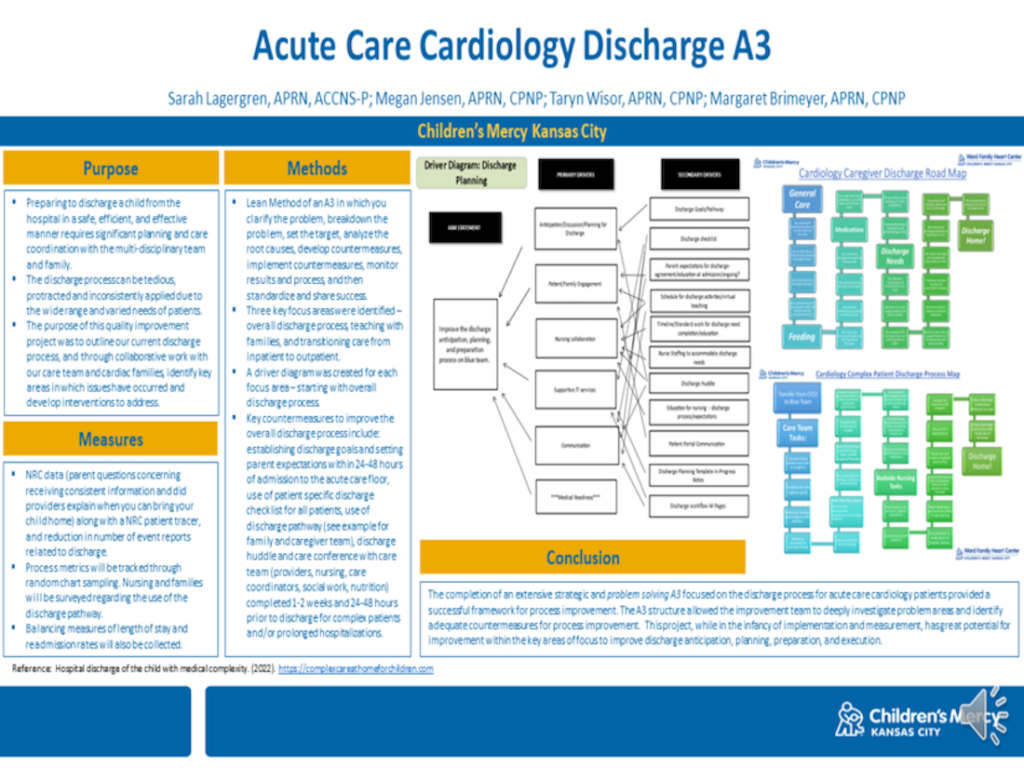
Children’s Mercy Hospital: Acute Care Cardiology Discharge A3
Sarah Lagergren, APRN, ACCNS-P Children’s Mercy Hospital, Kansas City
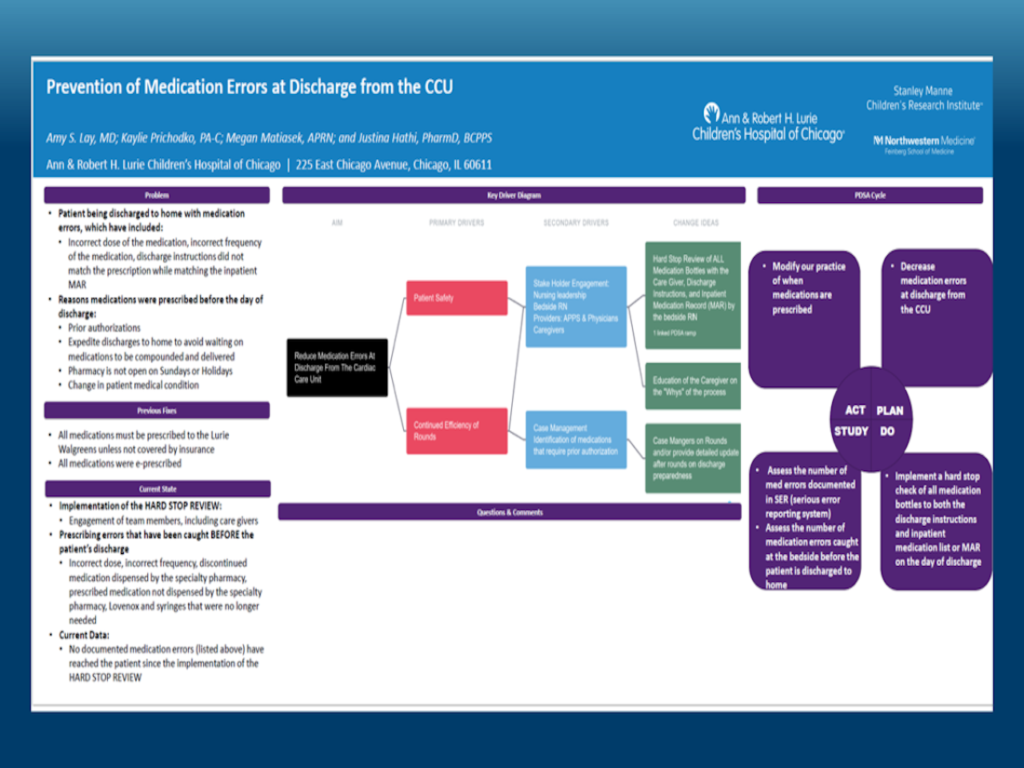
Prevention of Medication Errors at Discharge from the CCU
Amy Lay, MD Ann & Robert H. Lurie Children’s Hospital of Chicago
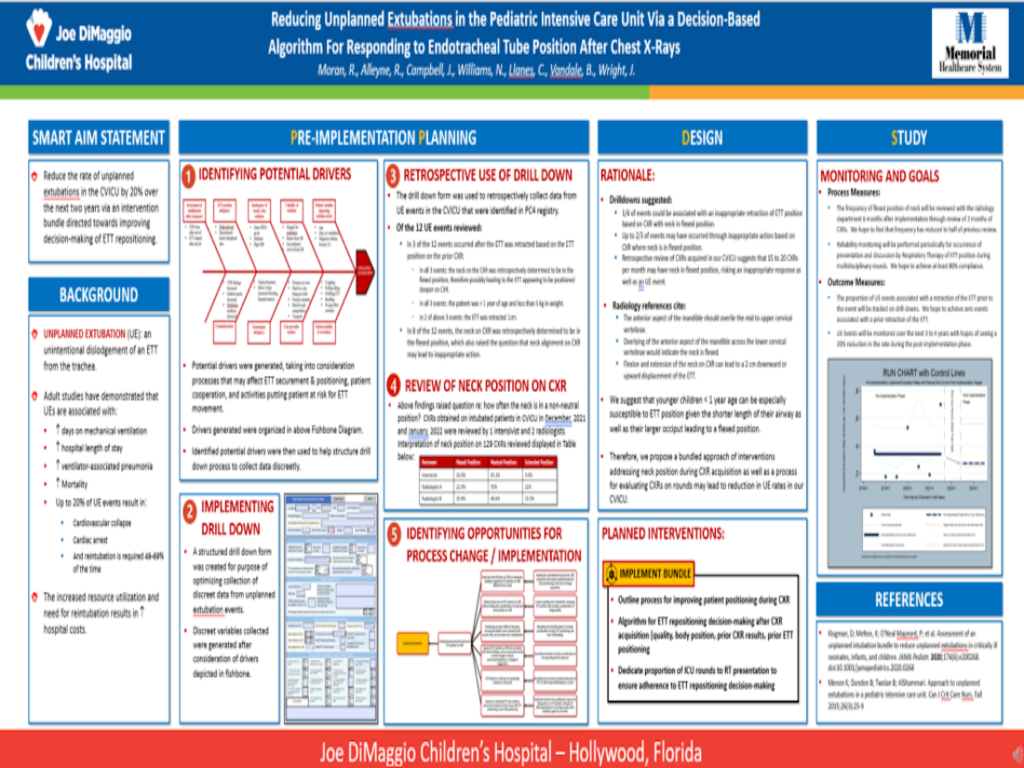
Reducing unplanned extubations in the Pediatric Intensive Care Unit via a decision-based algorithm for responding to Endotracheal tube position after chest x-rays
Ryan Moran, MD Memorial Healthcare System, Joe DiMaggio Children’s Hospital

Reducing unnecessary prescriptions at the time of discharge
Martha Nicholson, MD Lucile Packard Children’s Hospital at Stanford
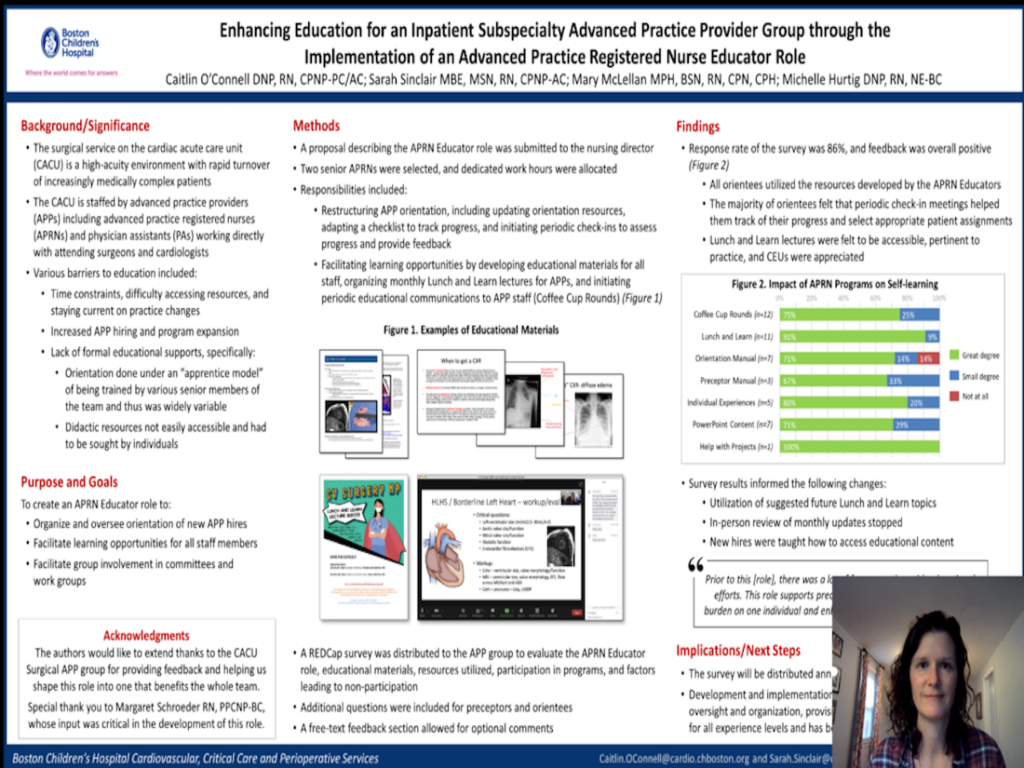
Enhancing Education for an Inpatient Subspecialty Advanced Practice Provider Group through the Implementation of an Advanced Practice Registered Nurse Educator Role
Caitlin O’Connell, DNP, RN, CPNP-PC/AC Boston Children’s Hospital

A single center perspective on standardized practices for Central Venous Catheter removal in Acute Care Cardiology
Megan Rodts, MD Cincinnati Children’s Hospital
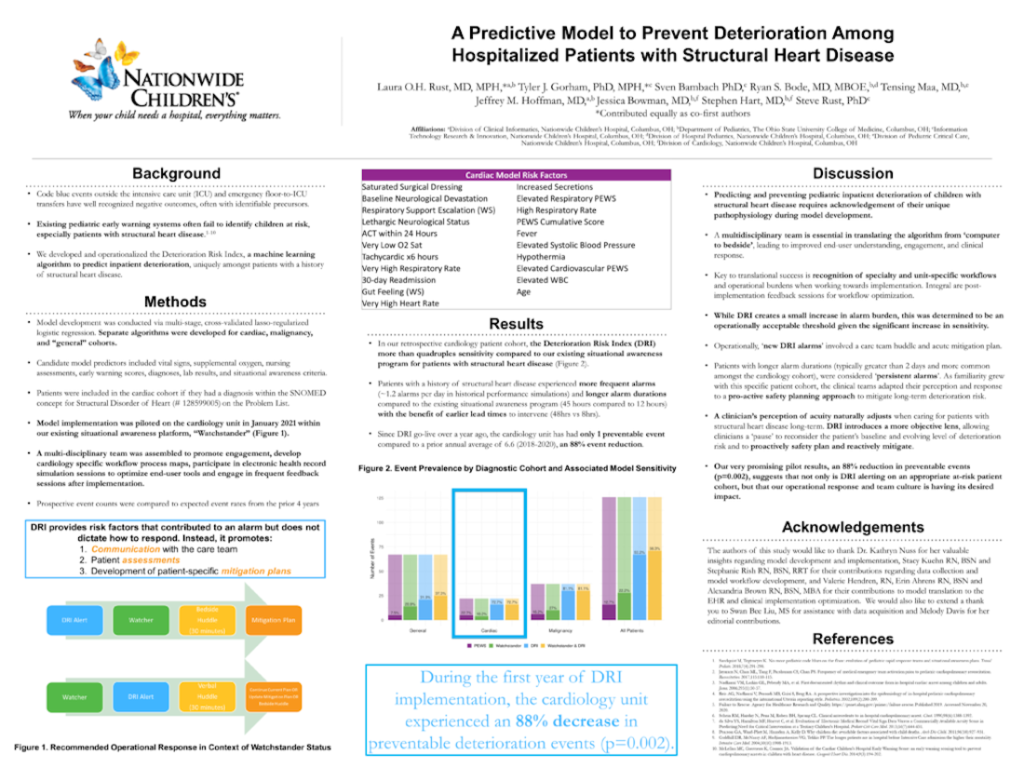
A predictive model to prevent deterioration among hospitalized patients with structural heart disease
Laura Rust, MD, MPH Nationwide Children’s Hospital
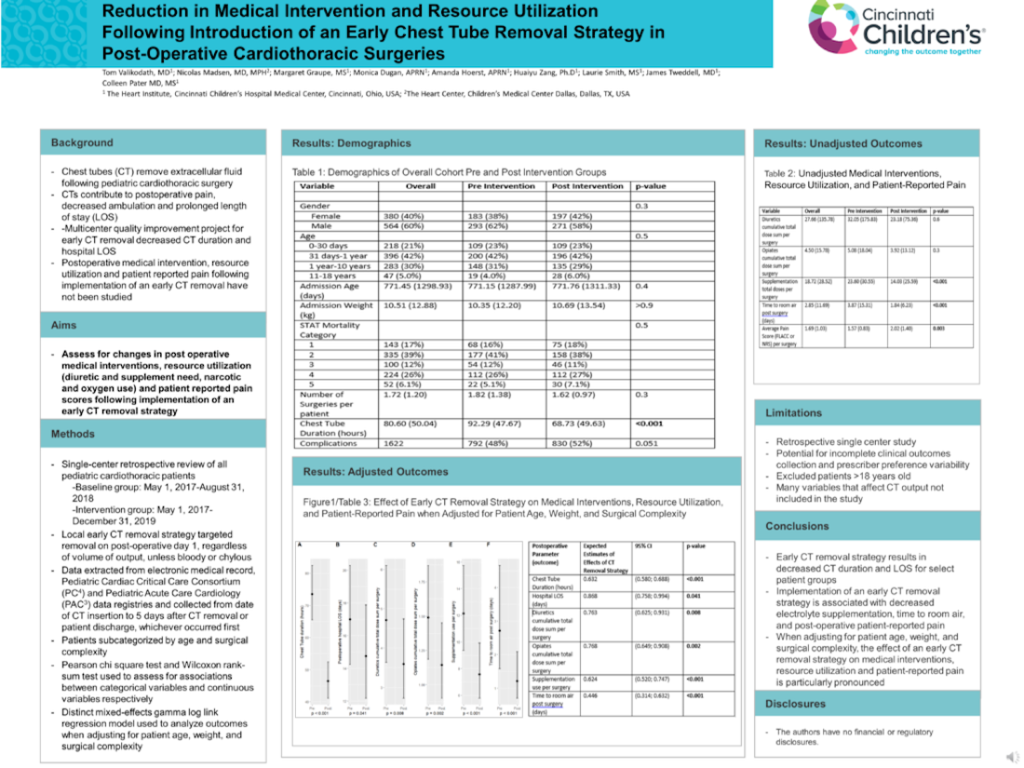
Reduction in medical intervention and resource utilization following introduction of an early chest tube removal strategy in post-operative cardiothoracic surgeries
Tom Valikodath, MD Cincinnati Children’s Hospital
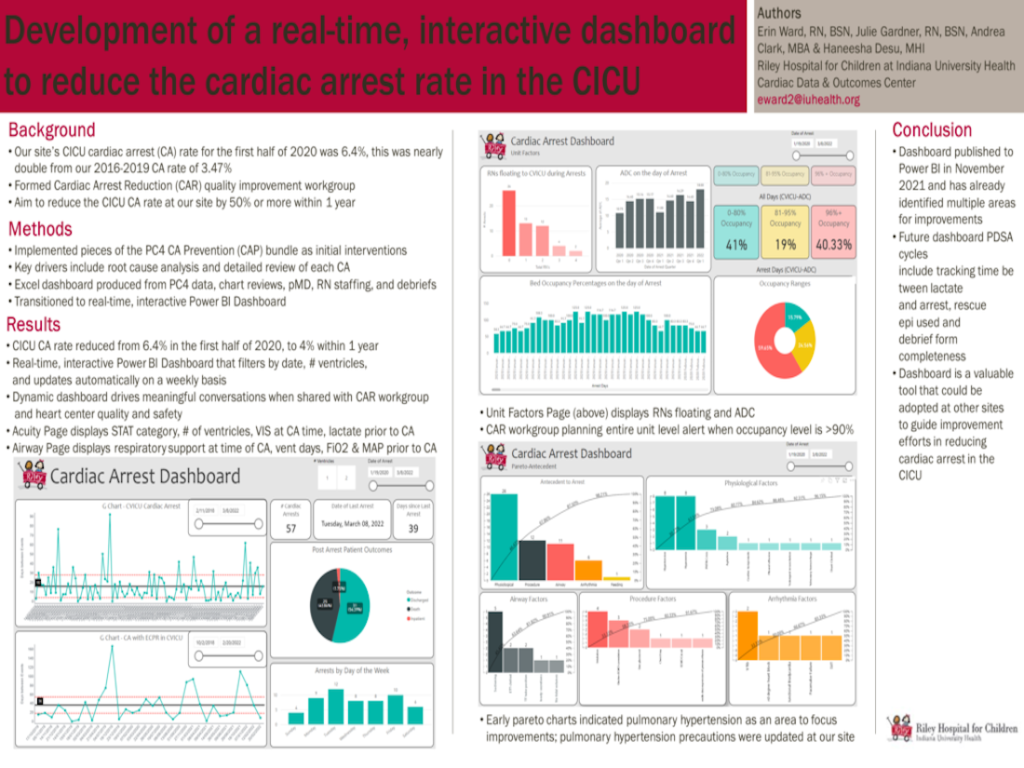
Development of a real-time, interactive dashboard to reduce the cardiac arrest rate in the CICU
Erin Ward, RN, BSN Riley Hospital for Children, Indiana University Health
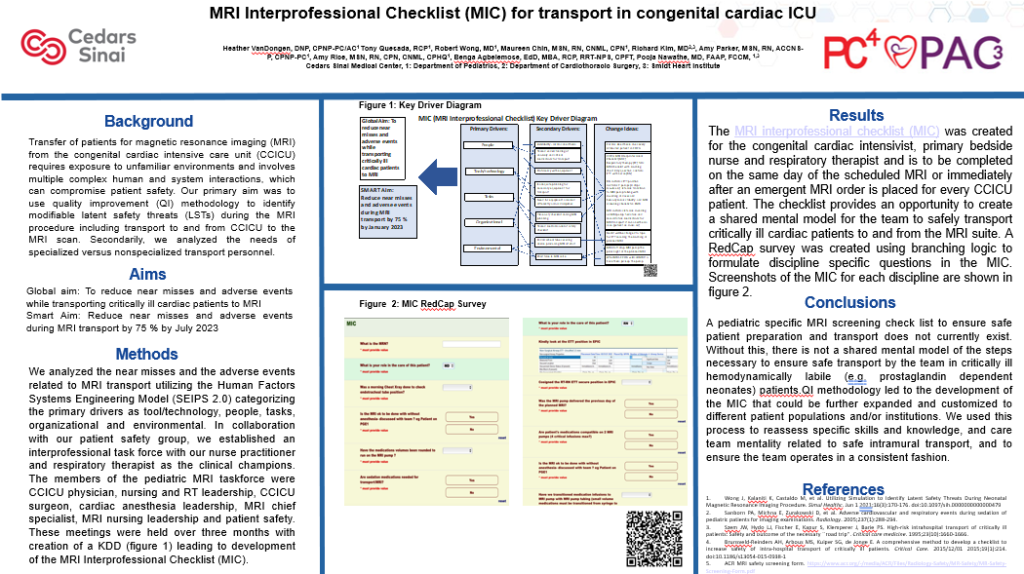
MRI Interprofessional Checklist (MIC) for transport in congenital cardiac ICU
Pooja Nawathe, MD, FAAP, FCCM Cedars Sinai Medical Center